Transforming Nursing Home Care Together (TNT) Program
 1st Place - 2023 Poster Session Winner
1st Place - 2023 Poster Session Winner
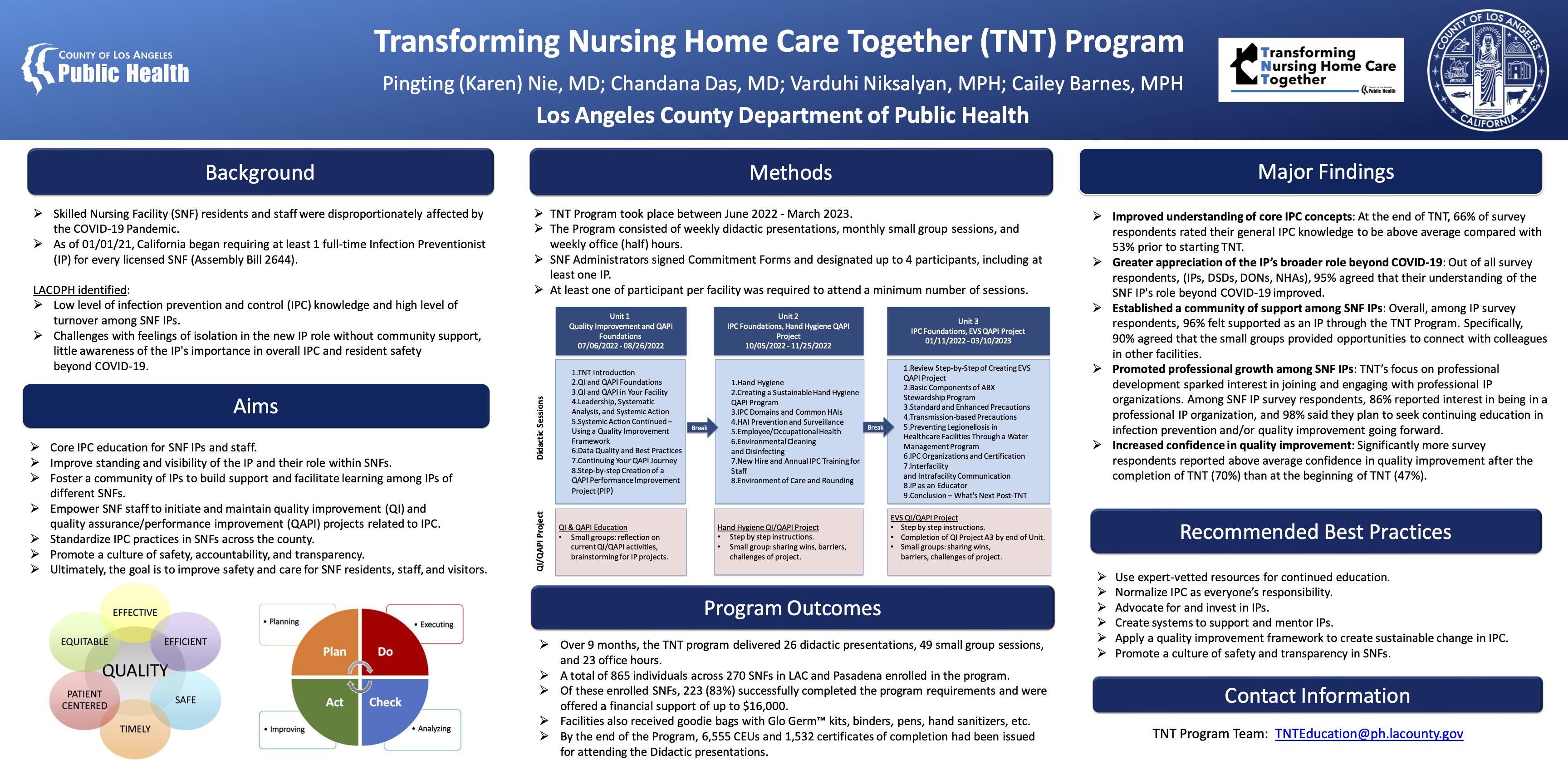
The Los Angeles County Department of Public Health (LAC DPH) ran a 9-month program called Transforming Nursing Home Care Together (TNT) between July 2022 and March 2023. The Program not only covered foundational quality improvement and infection prevention and control (IPC) content, but also aimed at fostering a culture of safety and accountability within skilled nursing facilities (SNFs). The Program focused on empowering Infection Preventionists (IPs), engaging SNF leadership from the corporate to the facility level, and teaching quality improvement concepts to make sustainable IPC change. LAC DPH aimed to make a lasting positive impact in the most populous county in the United States.
Background
Residents and staff of long-term care facilities, in particular skilled nursing facilities (SNFs), were disproportionately affected by the COVID-19 pandemic, accounting for 6% of cases and 40% of deaths in the United States by the end of November 2020.[i] While good infection prevention and control (IPC) practices may have prevented some cases and deaths from COVID-19 in this high-risk population, IPC requirements prior to the COVID-19 pandemic were quite modest and did not include a requirement for dedicated IPC staff.
On January 1, 2021, California Assembly Bill 2644 began requiring at least one full-time dedicated infection preventionist (IP) for every licensed SNF in the state, regardless of size.[ii] However, the LAC DPH long-term care facilities team observed that this important requirement initially had modest benefits, likely related to a low level of baseline knowledge and high level of turnover among SNF IPs. Additional challenges were identified, such as a feeling of isolation in the new IP role without a community of support; little awareness of the IP’s importance in overall IPC and resident safety beyond COVID-19; and little to no support from other facility leaders. When the Nursing Home and Long-term Care Facility Strike Team and Infrastructure Project grant was awarded by the CDC to LAC DPH in 2021[iii], the additional funding provided LAC DPH leadership an opportunity to address some of the IPC deficiencies identified in SNFs during the COVID-19 pandemic. LAC DPH leadership decided to focus the funding on training SNF IPs in order to increase their baseline IPC knowledge, improve their standing and visibility within SNFs, foster the creation of a community for IPs to facilitate learning among them, and standardize IPC practices across all of the SNFs in LAC.
Program Description
The TNT program consisted of three 2-month long units, composed of weekly didactic sessions. Participants viewed all presentations virtually on a web-based platform. The weekly didactic presentations were developed and delivered by subject matter experts within LAC DPH and collaborators from the California Department of Public Health (CDPH) and Health Services Advisory Group (HSAG). Along with weekly educational presentations, there were weekly open-format virtual office hours and monthly facilitated small group sessions. The first unit covered the fundamentals of quality improvement and a culture of safety. Units 2 and 3 went in-depth on core IPC topics, including healthcare associated infections, hand hygiene, standard and transmission-based precautions, environmental cleaning and disinfection, antimicrobial stewardship, and more.
To complete the program, facilities had to attend a minimum number of didactic presentations and small groups. Additionally, each facility was required to submit an IPC-related performance improvement project following an established quality improvement template called the A3. SNFs that met program requirements received a Certificate of Completion and financial support. Individual participants were eligible to receive Continuing Education Units (CEU) or certificates of completion, and CEUs earned in the TNT Program could count towards CDPH’s annual 10-hour requirement for IPs.
Program Outcomes and Major Findings
Over 9 months, the TNT program delivered 26 didactic presentations, 49 small group sessions, and 23 office hours. A total of 865 individuals, and 270 SNFs, in LAC and Pasadena enrolled in the program. Of these enrolled SNFs, 223 (83%) successfully completed the program requirements and were offered a financial support of up to $16,000. By the end of the program, 6,555 CEUs and 1,532 certificates of completion had been issued.
LAC DPH regularly conducted knowledge assessments and proactively gathered feedback over the course of the Program. This is a summary of major findings based on that feedback:
-
Improved understanding of core IPC concepts: At the end of TNT, 66% of participants rated their general IPC knowledge to be above average compared with 53% prior to starting TNT.
-
Greater appreciation of the IP’s broader role beyond COVID-19: Out of all survey respondents, including IPs, directors of staff development, directors of nursing, and nursing home administrators, 95% agreed that their understanding of the SNF IP's role beyond COVID-19 improved as a result of TNT.
-
Established a community of support among SNF IPs: Overall, 96% of IPs felt supported as an IP through the TNT Program. Specifically, 90% of participants agreed the small groups provided opportunities to connect with colleagues in other facilities.
-
Promoted professional growth among SNF IPs: TNT’s focus on professional development sparked interest in joining and engaging with professional IP organizations. Among SNF IP respondents, 86% reported interest in being in a professional IP organization, and 98% said they plan to seek continuing education in infection prevention and/or quality improvement going forward.
-
Increased confidence in quality improvement: Significantly more participants reported above average confidence in quality improvement after the completion of TNT (70%) than at the beginning of TNT (47%).
Recommended Best Practices
The TNT program identified several best practices for all SNFs, regardless of participation in TNT, to improve their IPC practices:
Use expert-vetted resources for continued education. LAC DPH’s TNT program materials are free and available to the public on LAC DPH’s TNT Website. SNFs inside and outside of LAC are invited to use these free resources that have been vetted by subject matter experts to provide IP-level education to their SNF staff, either as a standalone course or as a supplement. While LAC DPH is no longer issuing CEUs for post-program viewing of the didactic presentations, SNFs and other local health jurisdictions are encouraged to use the TNT Program materials to develop their own training and provide continuing education while acknowledging LAC DPH. Other training resources can also be found on the TNT Website.
Normalize IPC as everyone’s responsibility. Quality improvement and infection prevention are everyone’s responsibilities in a SNF. When launching and maintaining an IPC program in SNFs, all facility leadership roles need to be actively engaged on paper and in practice. This includes, but is not limited to, the director of nursing, director of staff development, nursing home administrator, and department supervisors or managers in dietary, laundry, maintenance, housekeeping, activities, social work, rehabilitation services, and more. Leadership plays a role in modeling by setting IPC as a priority, which directly impacts the behavior of all staff, including frontline workers.
Advocate for and invest in IPs. While IPC is a shared responsibility, proactive leadership support to train and retain IPs long-term will positively impact resident safety. Only 35% and 31% of IP respondents on TNT program surveys reported financial support for IPC education and increased compensation, respectively. Facility leadership, including nursing home administrators and corporate leadership, have an important role to champion both IPC programs and the IPs in their facilities by being actively engaged and allocating resources to IPC and quality improvement of IPC.
Create systems to support and mentor IPs. Beyond designating and training back-up IPs, facilities and SNF corporations should establish and foster committees, teams, or systems of support and mentorship for their IPs. Out of a sample of 143 IP participants in TNT, only 76% reported they have dedicated time for advanced education and training in IPC free from clinical responsibilities. A teamwork approach to IPs, as opposed to relying on a singular individual, not only provides basic necessities like coverage for sick days or vacations, but also encourages learning and career advancement that is ultimately beneficial to the whole facility and its residents.
Apply a quality improvement framework to create sustainable change in IPC. The TNT Program used the basic concept of the Plan, Do, Check/Study, Act (PDCA) cycle with the A3 quality improvement template to help SNF staff efficiently identify, investigate, and improve IPC practices. Quality improvement concepts and tools provide organization, consistency, teamwork, and a basis for new ideas to problem-solve. Facilities may choose more advanced frameworks or tools to meet their needs.
Promote a culture of safety and transparency in SNFs. Empower all SNF staff, including frontline workers, to share ideas and problem solve through the quality improvement process without fear of retribution or reprimand. Following a more horizontal teamwork approach instills a sense of ownership for resident outcomes and greater interdisciplinary collaboration, which ultimately help improve both resident and healthcare worker health and safety.
Click here to view poster.
Authors:
Pingting (Karen) Nie, MDChandana Das, MDVarduhi Niksalyan, MPHCailey Barnes, MPHReferences
[i] Kaiser Family Foundation. State data and policy actions to address coronavirus: COVID-19: metrics by state. San Francisco, CA: Kaiser Family Foundation; 2020. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/#long-term-care-cases-deaths
[ii] California Department of Public Health. All Facilities Letter 20-84: “Infection Prevention Recommendations and Incorporation into the Quality and Accountability Supplemental Payment (QASP) Program.” Published November 4, 2020: https://www.cdph.ca.gov/Programs/CHCQ/LCP/Pages/AFL-20-84.aspx
[iii] Centers for Disease Control and Prevention. “Nursing Home & Long Term Care Facility Strike Team and Infrastructure Project Guidance.” Released October 1, 2021: https://www.cdc.gov/hai/hai-ar-programs/activities/striketeam.html
